From Gut to Brain
The Silent Power of Microbes on Your Mood and Immunity
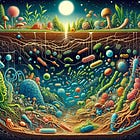
You may not feel them, see them, or even think about them—but trillions of microbes living in your gut are quietly shaping your mood, sharpening your mind, and training your immune system. These microscopic allies—or adversaries—form a complex communication network between your gut, brain, and immune cells, silently influencing everything from how you respond to stress to how effectively your body fights infection.
In recent years, science has revealed just how powerful this gut–brain–immune connection truly is. In this post, we explore the hidden world of your microbiome—and how caring for it might be the smartest health investment you make.
The Gut–Brain–Immune Superhighway: A Three-Way Conversation
Your gut isn’t just digesting your meals—it’s functioning as a high-speed communication hub, relaying constant updates to your brain and immune system. This tri-directional network, known as the gut–brain–immune axis, helps maintain balance across your mental state, immune defenses, and microbial ecosystem.
At the heart of this system are trillions of microbes residing in your intestines. They communicate with the brain through the vagus nerve, a kind of biological hotline, and also by releasing short-chain fatty acids (SCFAs) and neurotransmitter-like chemicals that affect mood, behavior, and cognition.
Over 70% of immune cells live in or near the gut and constantly respond to microbial signals. When your microbiome is balanced, the system runs smoothly. But poor diet, stress, or antibiotics can distort these signals, increasing inflammation, stress hormone levels, and your risk of anxiety or illness.
Mood in the Microbiome: How Bacteria Influence How You Feel
Gut microbes help produce neurotransmitters like serotonin, dopamine, and GABA—all crucial to emotional regulation. These microbes also affect your hypothalamic–pituitary–adrenal (HPA) axis, the body’s stress-response system.
Clinical studies back this up. A 2023 double-blind, randomized trial found that a probiotic blend of Bifidobacterium and Lactobacillus reduced depressive symptoms by nearly 25% in adults with major depression. Additional research confirms that probiotics and prebiotics—nutrients that support beneficial bacteria—can improve mood in people with mild to moderate symptoms.
On the flip side, dysbiosis—a microbial imbalance—can trigger the release of inflammatory compounds like lipopolysaccharides (LPS), which interfere with mood and brain function.
Think of your gut microbiota as a biochemical orchestra. When the right players are in tune and well-fed, the brain’s symphony is harmonious. When the balance is off, the whole system can fall out of rhythm.
Microbial Memory Boost: The Gut’s Surprising Role in Cognition
Gut microbes don’t just affect your mood—they also impact how you think and remember. Short-chain fatty acids (SCFAs) like butyrate can cross into the brain and support neurogenesis, the growth of new brain cells.
A 2022 study involving over 1,200 adults found that certain gut microbes predicted up to 20% of memory performance. Animal studies support this too—mice without gut bacteria had impaired memory, which improved when their microbiome was restored. Even early-stage human trials suggest that probiotic supplementation may enhance memory and concentration, particularly in older adults or those under stress.
In short, your gut microbes aren’t just helping you digest—they’re helping you think. Nourishing them may be one of the most brain-boosting habits you can adopt.
First Line of Defense: How Gut Microbes Train Your Immune System
Your gut is also the training ground for your immune system. More than 70% of immune cells live near or within the gut lining. Beneficial microbes help immune cells learn when to attack and when to hold back, reducing the risk of allergies, autoimmunity, and chronic inflammation. They help develop regulatory T cells, which calm inflammation and prevent overreactions like allergies or autoimmunity.
A healthy gut produces compounds like butyrate, which strengthen the gut lining and regulate immune signals. When this balance is lost—due to antibiotics or poor diet—the barrier weakens, allowing harmful substances like LPS to leak into the bloodstream, triggering chronic inflammation linked to asthma, diabetes, and even mood disorders.
One 2024 study found that patients taking a probiotic supplement experienced reduced levels of interleukin-6 (IL-6)—a pro-inflammatory marker—and increased immune-regulating T cells, suggesting gut microbes help restore both immune balance and mental health.
Balance or Breakdown: When Microbial Signals Go Wrong
When your gut microbiome is in balance, it acts like a finely tuned orchestra. But when harmful bacteria outnumber the good, the system begins to fail.
At the same time, helpful SCFA production declines, further weakening the gut lining and reducing supplies of mood-supporting chemicals like serotonin. The result is a vicious cycle: more inflammation leads to fewer good microbes, which leads to even more inflammation.
Symptoms such as brain fog, frequent infections, or anxiety may appear subtle, but they often signal a deeper microbial imbalance that, left unaddressed, can contribute to long-term health issues.
If you want to read related posts on Microbes, please read the following related posts:
Feeding Your Inner Allies: Everyday Steps to Support Your Microbiome
If your gut microbes are your health partners, then nourishing them is one of the best things you can do—no extreme diets or fancy supplements required. Just daily habits that support diversity and balance.
Eat more fiber (25–30 g/day from fruits, vegetables, legumes, and whole grains)
Include fermented foods (yogurt, kefir, kimchi, sauerkraut, miso)
Cut back on ultra-processed foods and added sugars
Add healthy fats (olive oil, flaxseeds, nuts, fatty fish)
Exercise regularly and prioritize sleep
Use antibiotics only when necessary
Manage stress through breathing, walking, or mindfulness
These small changes can significantly improve your microbial health—and in turn, your mental clarity, emotional stability, and immune strength.
Conclusion: Listen to What Your Gut Is Telling You
Your gut is more than a digestive system—it’s a living ecosystem that plays a critical role in shaping your mood, memory, and immune resilience. When its microbial community is balanced, it supports you in powerful, silent ways. When it’s not, the consequences echo through your body and mind.
The encouraging truth? You have control. Small, daily actions—like choosing fiber-rich foods, managing stress, and sleeping well—can feed the right microbes and shift your health trajectory.
Your health begins in your gut. Start listening.
Additional Reading
Doenyas, C., Clarke, G. & Cserjési, R. (2025). Gut–brain axis and neuropsychiatric health: recent advances. Scientific Reports 15, 3415. https://doi.org/10.1038/s41598-025-86858-3
Kenneth, J., et al. (2025). The gut microbiota-immune-brain axis: Therapeutic implications. Cell Reports Medicine 6(3): 101982. https://doi.org/10.1016/j.xcrm.2025.101982
Ni Lochlainn, M., et al. (2024). Effect of gut microbiome modulation on muscle function and cognition: the PROMOTe randomised controlled trial. Nature Communications 15, 1859 (2024). https://doi.org/10.1038/s41467-024-46116-y
Rathore, K., et al. (2025). The Bidirectional Relationship Between the Gut Microbiome and Mental Health: A Comprehensive Review. Cureus.17(3):e80810. https://doi.org/10.7759/cureus.80810 .
Toader, C., et al. (2024). Mind, Mood and Microbiota—Gut–Brain Axis in Psychiatric Disorders. International Journal of Molecular Sciences, 25(6), 3340. https://doi.org/10.3390/ijms25063340
Zhang, R., Ding, N., & Feng, X. (2025). The gut microbiome, immune modulation, and cognitive decline: insights on the gut-brain axis. Frontiers in Immunology, 16, 1529958. https://doi.org/10.3389/fimmu.2025.1529958